Can Stress Affect Your Heart? Yes, Here’s How.
Managing stress is a major investment in your heart health. Here are answers to the most common questions I get from patients.
by Caylin Cheney, Advanced Registered Nurse Practitioner
Key Takeaways
Stress is normal and the “fight or flight” response it triggers is vital to keep us safe from danger. But chronic stress can wear on the body, especially the heart, over time.
Long-term stress is bad for your heart because it can lead to high blood pressure, inflammation, plaque build up, and more.
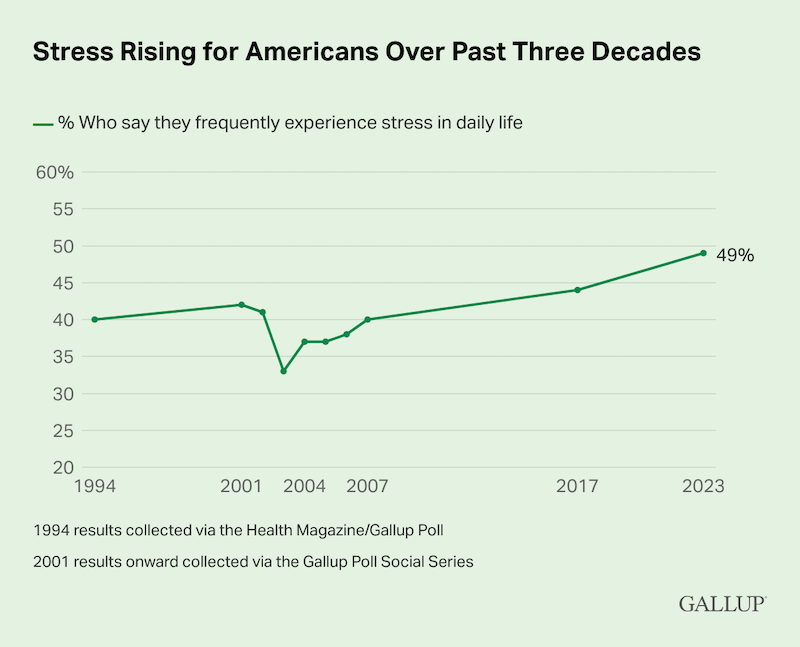
Nearly half of all adults in the U.S. report frequently feeling stressed, but there are many effective ways to reduce stress and improve your heart health.
This is the third blog in a series I’m writing about heart health. You can read straightforward explainers on blood pressure and cholesterol, too.
Stress-related heart attacks happen all the time in pop culture. Like Leo McGarry on West Wing, Phoebe in a weird alternate reality episode of Friends, and Jack Nicholson’s character in Something’s Gotta Give – just to name a few. And while the way heart attacks are portrayed in movies and TV aren’t usually accurate, you might be wondering if stress really can cause damage to your heart.
The answer is yes. Stress – particularly long-term, chronic stress – is, in fact, bad for your heart. And it often goes unrecognized as a major factor for conditions like heart disease!
I’ve been writing a series of explainers about heart health lately (including blogs on cholesterol and blood pressure), and I think it’s important to also connect the dots between stress and heart issues, too. Here are answers to some of the most common questions I hear from my patients:
What does stress do to the body?
All of us know what stress feels like when it hits. But what’s actually happening in our body when we get that “fight or flight” sensation?
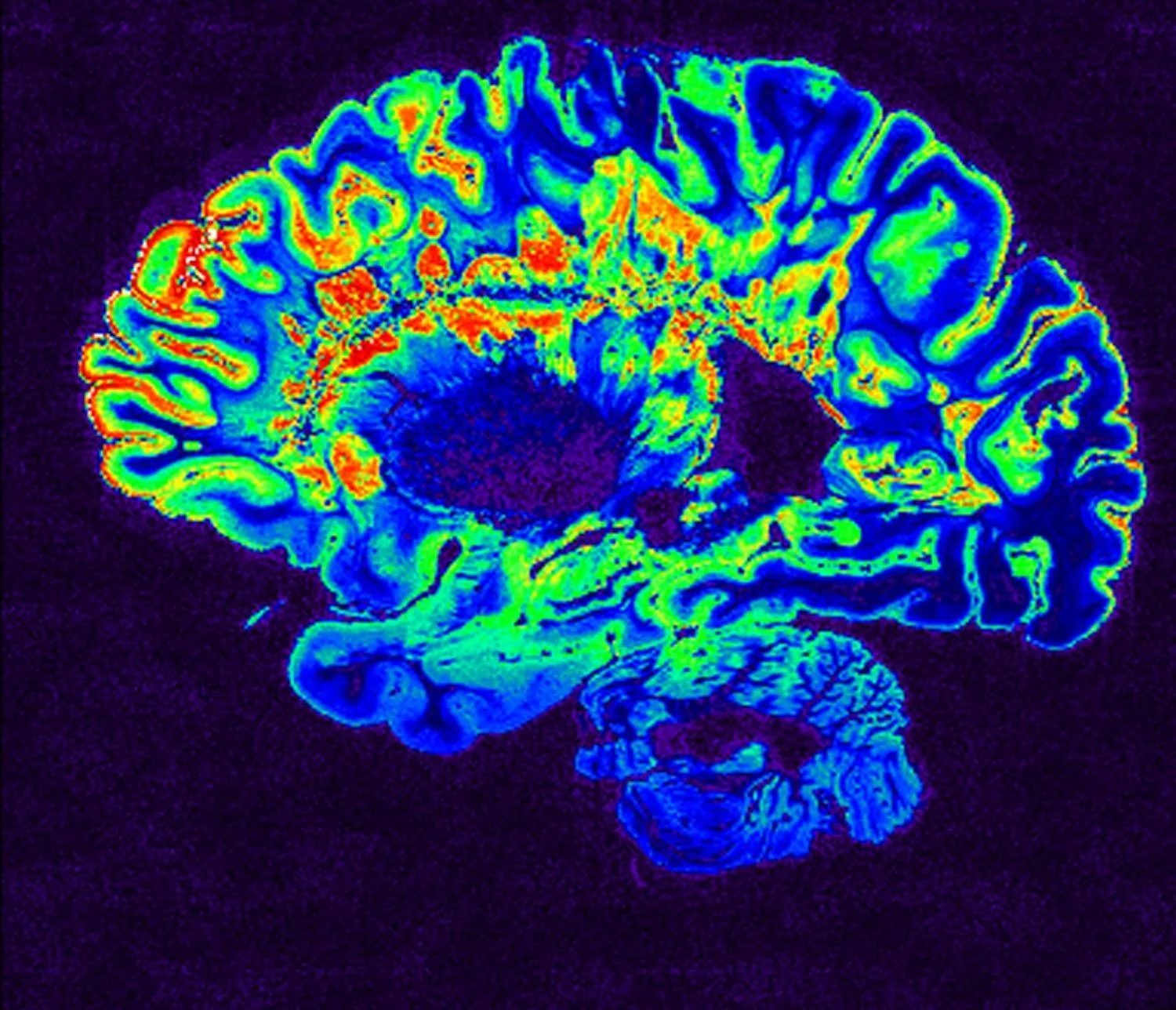
It’s a complex bodily response, but here’s a simplified version: When you experience something stressful, your brain sends a distress signal to the rest of your body through the hypothalamus – which is like a control center, in charge of all the things you do but don’t have to think about such as breathing or your heartbeat. That distress signal activates your sympathetic nervous system and your body begins to release adrenaline and cortisol to both kickstart the fight or flight response and maintain it.
That’s why when you’re stressed, you start to breathe faster, your heart feels like it’s racing, you feel energized, and your senses are sharpened. This is exactly how the system is designed to work in order to keep us safe from threats.
But chronic stress can put wear and tear on our bodies over time. We can’t keep our bodies in fight or flight mode all the time, just like we can’t run a car at 100 mph forever.
Why is stress bad for your heart?
Let’s zoom in on the heart impacts of stress, which are all a bit intertwined:
Blood pressure: In moments of stress, cortisol and adrenaline make your heart beat faster, but these hormones also constrict blood vessels – which leads to a spike in blood pressure. When you’re stressed long-term, you may develop chronic hypertension, a diagnosis for when a person consistently has high blood pressure that puts stress on the walls of their arteries. If left untreated, hypertension can cause damage to your heart and circulatory system (as well as your brain, kidneys, and eyes).
Inflammation: Cortisol released from long-term stress can also create inflammation in the body, including your arteries (the vessels that deliver blood to your body from your heart). Inflammation is a hot topic on social media right now and it can be hard to separate fact from fiction. But at its core, inflammation is an immune response. Inflammation can damage the inner lining of your arteries and cause plaque to accumulate and build up there.
Plaque build-up: As plaque builds up, the walls of your arteries harden and narrow. This restricts blood flow and increases the risk of heart disease, heart attacks, and stroke.
Indirect effects: Stress also can cause you to change your behavior and make it harder to prioritize the basics that help maintain good health. If you’re stressed, you might miss sleep, find it difficult to make time for physical activity, eat more processed food, drink more alcohol or smoke, etc. These are all factors that can increase your cholesterol or blood pressure, potentially with negative impacts for your heart.
What are the best ways to reduce stress?
First, I want to acknowledge that there are many deeply valid economic, social, and personal reasons to be stressed today – in fact, nearly half of adults in the U.S. say they frequently experience stress.
Reducing stress can look different for everyone! For me, I watch reruns of the Barefoot Contessa or Magnolia Table. I also love to throw a little living room dance party to "Hot Blooded" by Foreigner (my son loves it and I've created a dance party monster).
Here are just a few effective ways of reducing stress that I often recommend to my patients (including some of the wellness basics I’ve mentioned before!):
Prioritize sleep and establishing a consistent sleep routine
Minimize screen time, particularly right when you wake up and go to sleep
Move your body daily, aiming for about 150 minutes of a physical activity you enjoy each week
Stay hydrated, eat regularly, and eat as little processed food as you can
Try box breathing or meditation to help regulate your nervous system
Make time to practice your favorite hobbies and activities
Spend time with animals or in nature
Practice mindfulness and keep a symptom tracker
Make time to connect with people who are supportive, kind, and loving
Getting medical care shouldn’t be stressful
I started my own practice because I believe the way care is usually delivered leaves too many people feeling unheard, unseen, or overwhelmed.
My promise is that your experience, voice, and autonomy are not just respected here; they are the starting point for every decision we make together. I don’t offer one-size-fits-all treatment. I dedicate the time to understand the whole you, so we can move beyond just symptom management and truly get to the root of what's going on.
So if you’re looking for support to improve your heart health, get care for anxiety or depression, manage chronic conditions, or something else – schedule a visit today. I offer virtual visits for people across Washington state Monday through Friday, as well as in-person visits in Seattle on Wednesdays!